Getting to medical appointments can be tough, especially if transportation is a challenge. Ohio Medicaid offers Non-Emergency Medical Transportation (NEMT) to help eligible Cleveland families access healthcare. This guide explains how to:
- Check your Medicaid eligibility and confirm NEMT coverage.
- Use waiver programs like PASSPORT or MyCare Ohio for extra benefits.
- Gather required documents like your Medicaid ID and Physician Certification of Medical Necessity.
- Book rides with approved providers, including ReliaWheels.
- Solve common transportation issues and understand key rules.
Whether you need a wheelchair-accessible van or regular transport, this guide ensures you can navigate the process smoothly.
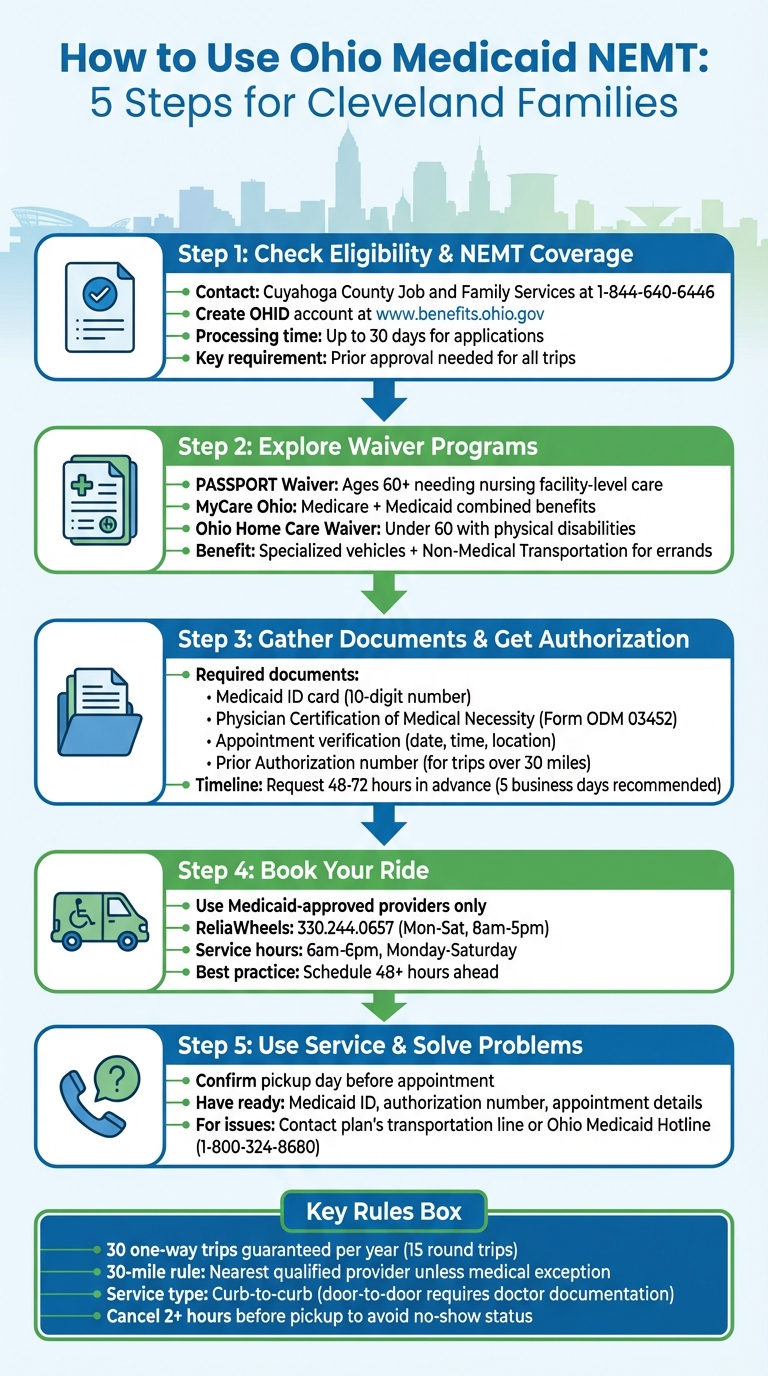
5-Step Process to Access Ohio Medicaid NEMT Services for Cleveland Families
Step 1: Check Your Medicaid Eligibility and NEMT Coverage
Medicaid Eligibility Requirements
If you're an Ohio resident with a Social Security number, you might qualify for Ohio Medicaid, provided you meet U.S. citizenship requirements or qualify under programs like Refugee Medical Assistance or Alien Emergency Medical Assistance.
Medicaid is designed to support low-income individuals, pregnant women, children, older adults, and those with disabilities. Your eligibility depends on your monthly income, which varies based on the program category - whether it's for children and families or for the aged, blind, or disabled. Residents in Cleveland can get personalized help by contacting Cuyahoga County Job and Family Services (CJFS) at 1-844-640-6446.
Even if you're unsure about your income eligibility, it's worth applying. The Ohio Department of Medicaid encourages everyone to apply, as applications can take up to 30 days to process. Once your documents are submitted, the system typically updates within five business days.
After confirming your Medicaid eligibility, the next step is to check if your plan includes Non-Emergency Medical Transportation (NEMT).
Verify NEMT Coverage in Your Plan
Most Ohio Medicaid plans offer free transportation for approved medical appointments. To confirm your NEMT coverage, you can create an OHID account through the Ohio Benefits Self-Service Portal at www.benefits.ohio.gov. For faster assistance, call the Eligibility Contact Center at 1-844-640-6446 - you'll need your zip code, Social Security number, and date of birth ready. If you're part of a Managed Care plan, reach out to the Medicaid Managed Care line at 1-800-324-8680 for details about NEMT services and provider networks.
When contacting Medicaid about NEMT services, have the rider's name, date of birth, and appointment details handy, including the doctor's name, address, and phone number. Keep in mind that trips must be approved in advance by the Department of Job & Family Services. Without prior approval, you might need to cover the transit fare yourself.
Once you've confirmed your eligibility and NEMT coverage, you're ready to explore how Medicaid waiver programs can expand your transportation options.
Non-Emergency Medical Transportation (NEMT) Coordination Topics #4 of 4 (Apr. 13, 2022)
Step 2: Learn About Waiver Programs for Additional NEMT Benefits
Once your Medicaid eligibility is confirmed, it’s time to look into waiver programs that can expand your transportation options.
What Are Waiver Programs?
Ohio Medicaid waiver programs, also known as Home and Community-Based Services, are designed to support individuals with disabilities or chronic conditions who require nursing facility-level care but prefer to stay at home. These programs also include expanded transportation benefits.
- PASSPORT Waiver: This program is for Ohio residents aged 60 and older who need nursing facility-level care. The Western Reserve Area Agency on Aging (WRAAA) can help start the screening process for PASSPORT eligibility.
- MyCare Ohio: A managed care program for individuals who qualify for both Medicare and Medicaid. It combines all benefits under one plan, often simplifying scheduling and offering a broader range of providers.
- Ohio Home Care Waiver: Geared toward individuals under 60 with physical disabilities or complex medical needs, this program helps them access specialized services.
To qualify for these programs, you’ll need to complete a Level of Care (LOC) assessment. This involves a registered nurse or social worker visiting your home to evaluate whether you meet the medical and functional criteria for nursing facility-level care. These programs go beyond standard NEMT benefits, offering customized transportation solutions.
How Waiver Programs Help with NEMT
Waiver programs significantly expand transportation options beyond the standard Non-Emergency Medical Transportation (NEMT) benefits offered by Medicaid. While traditional NEMT covers rides strictly for medical appointments, waiver programs can include vehicles equipped for specialized needs, such as stretcher-capable or bariatric-equipped vans. Some waivers also provide Non-Medical Transportation (NMT) for essential errands like grocery shopping or pharmacy visits.
Once enrolled in a waiver program, you’ll work with a case manager who coordinates your transportation. They’ll ensure the vehicle is suited to your needs and can even authorize recurring trips for ongoing services like dialysis or physical therapy, saving you from needing repeated approvals. If you’re booking with ReliaWheels, make sure to mention your waiver program, such as MyCare Ohio or PASSPORT, to confirm provider authorization. MyCare Ohio members should also review their handbook for details on additional trips or extended mileage limits.
Step 3: Collect Required Documents and Get Prior Authorization
Make sure you have all the necessary documents and approvals to avoid any delays with your ride.
Documents You'll Need for NEMT
The most critical document is your Medicaid ID card. This card, issued by Ohio Medicaid or your Managed Care Organization (MCO) - such as CareSource, Buckeye Health Plan, or UnitedHealthcare - contains a 10-digit ID number that confirms your eligibility when booking or boarding a ride.
If you require specialized transportation, like a wheelchair-accessible van or stretcher service, you'll need a Physician Certification of Medical Necessity (PCM), typically Form ODM 03452. This form, signed by your doctor, physician assistant, or nurse practitioner, explains why public transportation or a personal vehicle isn't an option due to your medical condition. Request this form from your healthcare provider at least one to two weeks before your first ride to allow for processing time.
You'll also need proof of your medical appointment, which should include the date, time, location, and the name of your healthcare provider. Most medical offices can provide this documentation when you schedule your visit. For certain trips - especially those over 30 miles or to specialists outside Cuyahoga County - you may need a Prior Authorization (PA) number from your MCO or county agency. If you're part of a waiver program like PASSPORT or Ohio Home Care Waiver, make sure you have a copy of your Individual Service Plan (ISP) or authorization from your case manager.
| Document Type | Purpose | Key Detail to Check |
|---|---|---|
| Medicaid ID Card | Verifies membership and plan type | Ensure the 10-digit ID is active |
| Physician Certification (PCM) | Proves medical need for specialized transport | Must be signed by a doctor, PA, or NP |
| Appointment Verification | Confirms destination is a medical provider | Includes date, time, and suite number |
| Prior Authorization Form | Grants official approval for certain trips | Check for expiration dates on recurring trips |
Once your documents are ready, the next step is to secure prior authorization.
How to Get Prior Authorization
For managed care plans, call the transportation number on the back of your member ID card. If you're on fee-for-service Medicaid, contact the Cuyahoga County Department of Job and Family Services. Plan ahead by scheduling your rides 48–72 business hours in advance, though it's best to submit your request five business days before your appointment to avoid any last-minute issues.
Before you call, have a trip sheet prepared with essential details: your Medicaid ID, the name and NPI of your destination doctor, your appointment time, and the medical reason for your visit. You'll also need to fax or upload the signed PCM form. Once your request is processed, you'll receive a confirmation within a few days. Be sure to share your authorization number with your NEMT provider when you schedule the ride.
To avoid common errors, double-check that your forms are up-to-date, your contact information is accurate, and any special equipment needs - like wheelchair lifts or oxygen storage - are clearly noted. With your authorization number in hand, you're all set to book your ride with an approved provider.
sbb-itb-a0ce227
Step 4: Book Your Ride with Approved Cleveland Providers Like ReliaWheels
Once you've secured prior authorization, the next step is to book your ride. Make sure to schedule with a Medicaid-approved provider to stay within the program’s guidelines.
Find Medicaid-Approved NEMT Providers
Booking through a Medicaid-approved provider is essential - if you don't, you might end up covering the entire cost yourself. To find an updated list of approved providers, reach out to your Managed Care Organization (MCO) or the Cuyahoga County Department of Job and Family Services.
It’s also important to choose a provider with a dependable track record. This helps minimize the risk of service issues. Look for companies that are familiar with the local healthcare system and can meet specific needs, such as wheelchair access or stretcher transport.
Once you’ve identified a reliable provider, you’re ready to move forward with scheduling your ride, including with providers like ReliaWheels.
How to Schedule with ReliaWheels
To book a ride with ReliaWheels, call 330.244.0657 during their office hours - Monday through Saturday, 8:00 a.m. to 5:00 p.m. - or use the online Ride Request Form on their website. Be prepared with the following details when booking: your Medicaid ID, authorization number, appointment information (date, time, provider's name and contact), and any special equipment needs.
While ReliaWheels can often handle same-day ride requests, it’s best to schedule at least 48 hours in advance to guarantee availability. Their transportation services run Monday through Saturday, from 6:00 a.m. to 6:00 p.m., offering pickups across Northeast Ohio and transportation throughout the state.
If you’re part of a Managed Care plan, don’t forget to contact your plan’s transportation line either before or after booking with ReliaWheels.
Step 5: Use NEMT Services and Solve Common Problems
Be prepared for your ride and know how to tackle any issues that come up along the way.
Get Ready for Your NEMT Ride
The day before your ride, confirm your pickup time to avoid any scheduling mishaps. Make sure you have your Medicaid ID, authorization number, and appointment details handy to present to the driver when they arrive.
If you require special equipment, double-check these arrangements with your transportation provider. For example, Cleveland residents using ReliaWheels can count on their wheelchair-accessible vehicles and stretcher transport options, which are tailored for individuals with mobility challenges.
Save all important contact numbers (from earlier in the guide) so you’re prepared to deal with any unexpected situations. Once you're set, here's how to handle common problems that might arise during your ride.
Handle Common NEMT Problems
If your driver is running late or doesn’t show up, call your plan’s transportation line right away to report the issue and request a replacement ride. Cleveland residents who are not part of a managed care plan should contact the Cuyahoga County Department of Job and Family Services to speak with the Medicaid Transportation Coordinator.
When reporting an issue, have key details ready, such as your authorization number, pickup time, and appointment information. If you’re unable to resolve the problem through your plan, you can use the Ohio Medicaid Hotline (1-800-324-8680) as a backup resource for assistance, no matter your plan type.
For disputes that remain unresolved with the transportation provider, escalate the matter to your Managed Care plan’s member services or the state hotline to file a formal complaint. If you’re not in a managed care plan and require wheelchair van services, you can also contact approved providers directly to address scheduling conflicts.
| Your Coverage Type | Who to Contact for Problems | Phone Number |
|---|---|---|
| Managed Care (CareSource) | CareSource Member Services | 1-800-488-0134 |
| Managed Care (Buckeye) | Buckeye Health Plan | 1-866-246-4358 |
| Managed Care (Molina) | Molina HealthCare | 1-800-642-4168 |
| MyCare Ohio (CareSource) | CareSource MyCare | 1-855-475-3163 |
| Not in Managed Care | Cuyahoga County Department of Job and Family Services (local office) | Contact local office |
| General Support | Ohio Medicaid Hotline | 1-800-324-8680 |
Ohio Medicaid NEMT Rules and Cleveland Resources
Important NEMT Rules to Know
Ohio Medicaid's Non-Emergency Medical Transportation (NEMT) program is designed to ensure access to healthcare appointments when transportation is a barrier. Coverage is strictly for Medicaid-approved services like doctor visits, dental appointments, therapy sessions, or pharmacy trips. It doesn’t extend to personal errands, grocery shopping, or social activities.
To schedule a ride, plan ahead: two business days for standard trips and three business days for wheelchair-accessible or stretcher transport. Managed Care Organizations (MCOs) in Ohio guarantee 30 one-way trips per member annually (equivalent to 15 round trips). If you exceed this limit, the Cuyahoga County Department of Job and Family Services steps in to arrange additional transportation for Fee-for-Service Medicaid members.
The "30-mile rule" means Medicaid covers rides only to the nearest qualified provider unless your doctor provides a medical reason for visiting a provider farther away. If your chosen provider is over 30 miles from your location, a referral from your physician is required. Standard NEMT services are "curb-to-curb", but if you need extra assistance - like help with stairs or entering a building - your doctor must document this need in advance for "door-to-door" or "door-through-door" service.
For help navigating these rules, Cleveland offers several local resources to make the process smoother.
Cleveland Support Resources
If you’re unsure about any of these guidelines, Cleveland-based support can help. For general questions about your NEMT benefits, call the Ohio Medicaid Consumer Hotline at 1-800-324-8680. The Cuyahoga County Department of Job and Family Services manages Medicaid eligibility and provides "County Transportation" services for members not enrolled in an MCO or for trips that MCOs don’t cover.
When arranging transportation, be prepared with your Medicaid ID number, the date and time of your appointment, and the full address of your medical provider. This ensures a smooth scheduling process and avoids unnecessary delays.
Additionally, ReliaWheels works with Cleveland families to provide specialized vehicles, including wheelchair-accessible and stretcher-equipped options. If your transportation needs are approved by Medicaid, ReliaWheels ensures you can travel safely and comfortably to your medical appointments.
Conclusion
Accessing Ohio Medicaid NEMT services can be a smooth process when you follow the necessary steps. Start by confirming your eligibility and gathering the required documents, such as your Medicaid ID and a Physician's Certification of Medical Necessity. Be sure to secure prior authorization at least 48 to 72 hours before your appointment to avoid any last-minute issues.
Scheduling your rides in advance is crucial. Most Ohio NEMT providers require reservations between 2 and 12 business days ahead of time. Additionally, make sure to cancel any rides you can’t take at least 2 hours before the scheduled pickup to avoid being marked as a no-show, which could temporarily suspend your benefits.
ReliaWheels is a trusted provider, offering reliable, on-time transportation with specialized vehicles for wheelchair or stretcher needs. This service is especially vital for Cleveland families attending appointments at Cleveland Clinic, University Hospitals, and other healthcare facilities in the area.
For assistance, the Cuyahoga County Department of Job and Family Services and the Ohio Medicaid Consumer Hotline at 800-324-8680 are available to help with questions or scheduling. By choosing approved providers and adhering to program rules, you can access dependable, no-cost transportation for your medical appointments, ensuring you receive the care you need without added stress.
FAQs
How can I check if I qualify for Ohio Medicaid NEMT services?
To find out if you're eligible for Ohio Medicaid NEMT (Non-Emergency Medical Transportation) services, the first step is to confirm your Medicaid eligibility. Basic requirements include being a U.S. citizen or an eligible non-citizen, meeting low-income guidelines, and living in Ohio. You can apply for Medicaid through the Ohio Benefits website or by reaching out to your local County Department of Job and Family Services.
After enrolling, make sure you have full Medicaid coverage and need transportation for medically necessary appointments. If you're unsure about your eligibility or need more information, call the Medicaid Hotline at 1-800-324-8680 for guidance.
What information and documents do I need to schedule a ride with Ohio Medicaid NEMT?
To book a ride with Ohio Medicaid's Non-Emergency Medical Transportation (NEMT) services, you’ll need to have a few key details ready:
- Your full name
- Date of birth
- Medicaid or Social Security number
- Your current residential address
- A phone number where you can be reached
In some cases, you might also need to complete and sign an authorization form. Certain forms may require a physician’s signature, so it’s worth checking with your healthcare provider or local Medicaid office to make sure you’ve got everything sorted before scheduling your ride.
How can programs like PASSPORT help with transportation needs?
Programs like PASSPORT offer a way to broaden transportation options by covering non-emergency medical transportation (NEMT) services through Medicaid. This program is specifically designed for eligible Ohio residents, particularly older adults, to help them remain in their homes and communities while accessing crucial services like healthcare.
With the help of a case manager, participants receive personalized care plans that can include transportation to medical appointments. This makes it easier to get to necessary healthcare services, removing obstacles that might otherwise hinder independence. By providing this kind of tailored assistance, PASSPORT ensures participants stay connected to essential resources, enhancing their ability to live independently and maintain a better quality of life.
.png?width=2931&height=601&name=Purple%20and%20Green%20Paper%20Music%20Event%20Banner%20(7).png)




